November 14, 2016
Medscape Medical News
Time for a U-turn on Levothyroxine? Overuse Is Rife, Say DocsLiam Davenport
Using levothyroxine to treat subclinical hypothyroidism
should be considered on a patient-by-patient basis and be started only after at least two thyroid-stimulating-hormone (TSH) tests show an abnormal result, urge a group of clinicians concerned about overuse of the drug.
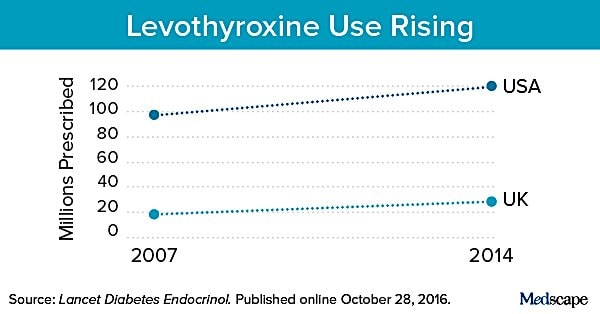
There has been an explosion in prescriptions for levothyroxine in recent years, largely driven by guidelines recommending the treatment of subclinical increases in TSH levels even in the absence of symptoms, they say.
However,
there is scant evidence to support a benefit from treatment, which may expose patients to ongoing out-of-pocket expenses, as well as adverse effects, particularly in older patients with naturally higher TSH levels."There is substantial uncertainty and complexity associated with the technical aspects of identifying otherwise-healthy people affected by mild, nonspecific symptoms who would benefit from levothyroxine," write René Rodriguez-Gutierrez, MD, knowledge and evaluation research unit, division of endocrinology, diabetes, metabolism, and nutrition, Mayo Clinic, "This uncertainty and complexity calls for policies that invite patients and clinicians to enroll in clinical trials to assess the effectiveness of levothyroxine use, rather than to the routine, expanding, and prolonged use of a treatment of uncertain value," they state.
Dr Rodriguez-Gutierrez told Medscape Medical News that he and his colleagues want to "call attention" to the issue of levothyroxine overuse.
As well as recommending that physicians adopt a precautionary, patient-centered approach when considering starting someone on the drug, it is also important that patients understand what is driving these prescriptions and "be more aware," he said, adding that in addition it's vital that the scientific and research community realize "that we have to do something."
"In the meantime, decisions still have to be made," Dr Rodriguez-Gutierrez noted. Involving the patient in the discussion "to see not only the benefits, of which we are not very sure, but also the harms and the costs and inconvenience" is key, and then a decision can be taken together as to whether to test and ultimately treat.
Levothryoxine Most Prescribed Drug in the USWhile the prevalence of overt hypothyroidism is low, at between 0.2% and 2.0% of the population, and its incidence is stable, the authors point out that the number of prescriptions for levothyroxine have increased substantially in recent years, and it is now the most prescribed drug in the United States, with 120 million prescriptions written in 2014, and the third most prescribed drug in the United Kingdom.
Several factors have driven the increase in prescriptions, the doctors say.
Subclinical hypothyroidism affects up to 12% of the adult population, and current guidelines say that those with TSH of ≥10 mlU/L, or those with TSH between 5.5 and 10 mlU/L who have potentially related symptoms, positive autoantibodies, or cardiovascular disease, should receive treatment.
Yet the guidelines are not backed up by data — the doctors argue there is a lack of evidence to suggest that there is a clear benefit of levothyroxine therapy outside of patients with thyroid cancer.
Adding to the pressure, the researchers note that the American Thyroid Association recommends that asymptomatic men and women aged over 35 years should be screened for thyroid dysfunction every 5 years, which has led to a "surge" in thyroid tests.
As a result, the proportion of patients being treated has increased in recent years, they state. In the United Kingdom, for example, those with TSH of 10 mlU/L or lower were prescribed levothyroxine 1.3 times more in 2009 than in 2001, and 31% of treated patients had normal thyroxine values and no symptoms or abnormal cardiovascular risk factors.
But the doctors point out that elevated
TSH levels normalize in around 60% of cases without intervention, potentially due to normal variations in TSH levels, the passing of a concomitant illness, concomitant drug use, and environmental and stress factors, among other things. In addition, healthy elderly people have been shown to have naturally higher TSH levels.Another issue is that
the symptoms of both subclinical and overt hypothyroidism, such as dry skin, hair loss, constipation, myalgia, and fatigue, are nonspecific and linked to hypothyroidism in only around 10% of cases."Therefore, symptoms might not reliably identify those who can benefit from levothyroxine treatment," the team writes.
Before prescribing levothyroxine, clinicians should also consider the financial implications, as the 3-month out-of-pocket cost to patients in the United States can be as high as $100, and treatment will result in ongoing clinical visits and possibly lifelong monitoring and follow-up.
Finally, levothyroxine is not without potential therapeutic consequences, they add.
In older patients with naturally higher TSH levels, treatment can result in adverse effects such as hyperthyroidism, increasing the risk of arrhythmias, angina pectoris, bone loss, and fractures, they observe.Repeat TSH Before Considering Treatment and Conduct More Studies
To improve the quality of levothyroxine prescription, the authors recommend several strategies, beginning with assessing the potential benefit vs burden of treatment on an individual patient basis.
They also recommend that, due to the potential for TSH levels to normalize over time, all patients with abnormally high TSH concentrations that are consistent with subclinical hypothyroidism should have the test repeated, ideally in the same laboratory, after 3 to 6 months before treatment is considered.
Moreover, it should be recognized that "patients with nonspecific symptoms and normal thyroid-function tests do not benefit from levothyroxine therapy."
If such treatment is started, the authors recommend that the lowest dose of a generic preparation of levothryoxine should be used and reassessed periodically to determine its efficacy.
In the meantime, the authors call for "much-needed research" on the efficacy of levothyroxine. Dr Rodriguez-Gutierrez explained that "what we need now is a pragmatic comparative-effectiveness study."
He said: "The idea would be to have a multicenter study," with different clinical scenarios, "including people with subclinical hypothyroidism, and then give them the treatment and see what happens on outcomes that matter to them.
"The outcome that matters to them is not TSH, it's quality of life," he stressed.
Such a study "will require an enormous effort from probably multiple researchers," he concluded.
The authors report no relevant financial relationships.
For more diabetes and endocrinology news, follow us on Twitter and on Facebook.
Lancet Diabetes Endocrinol 2016. Published online October 28, 2016. Editorial
Δεν είναι ορατοί οι σύνδεσμοι (links).
Εγγραφή ή
Είσοδος